Oh I would recommend him in a heartbeat, he does a good job, he's gentle, he explains everything to you, his bedside manner is great. He cares! ♥

Understand cataract surgery and how it works is important. Knowing the process results in high successful outcomes and the lifestyle you want.
TOPICS YOU WILL FIND ON THIS PAGE
If you live long enough you will develop a cataract. This is when the internal eye lens becomes cloudy and hard. Cataracts can develop from normal aging, from an eye injury, or if you have taken medications known as steroids. Cataracts may cause blurred vision, dulled vision, sensitivity to light and glare, and/or ghost images. If vision changes interferes with your daily life, the cataract may need to be removed. Cataract surgery is the only way to remove a cataract. You can decide not to have the cataract surgery, your vision loss from the cataract will continue to get worse.
Correcting the decreased vision and lessen your dependency on glasses or contact lens is the goal of cataract surgery. During the surgery, Dr. Aaron J. Affleck (the ophthalmologist or eye surgeon) removes the cataract and puts in a new artificial lens called an intraocular lens or IOL. The IOL will be left in the eye permanently. Cataract surgery will not correct other causes of decreased vision, such as glaucoma, diabetes, or age-related macular degeneration. At Affleck, M.D. Eye Care we strongly recommend using an advanced IOL (PanOptix). Most people who do not still need to wear glasses or contact lens after cataract surgery for either near and/or distance vision and astigmatism.
If you agree to have the surgery, you will undergo a personalized complete eye examination by Aaron J. Affleck, M. D. This may include an examination to determine your eyeglass prescription (refraction), measurement of your vision with and without glasses (visual acuity), measurement of the pressures inside your eye (tonometry), measurement of the curvature of your cornea (keratometry), ultrasonic measurement of the length of your eye (axial length), intraocular lens calculation (biometry) to determine the best estimate of the proper power of the implanted IOL, microscopic examination of the front part of your eye (slit-lamp examination), and examination of the retina of your eye with your pupils dilated.
Dr. Affleck goes beyond the standard test requirements to ensure the most accurate calculations/measurements.
Stop wearing rigid (including gas permeable and standard hard) contacts lenses for at least six weeks before receiving measurements for your IOL and before cataract surgery. If you wear soft contact lenses ask Dr. Affleck how long to stop wearing them before measurements and surgery.
If you wear rigid or hard contact lenses, you must leave them out of your eyes for a period of time before your preoperative eye examination and before your surgery. This is done because the contact lens rests on the cornea and distorts its shape, which can effect the accuracy of the measurements of the IOL power. When you stop wearing your contact lenses, the corneas can return to their natural shape.
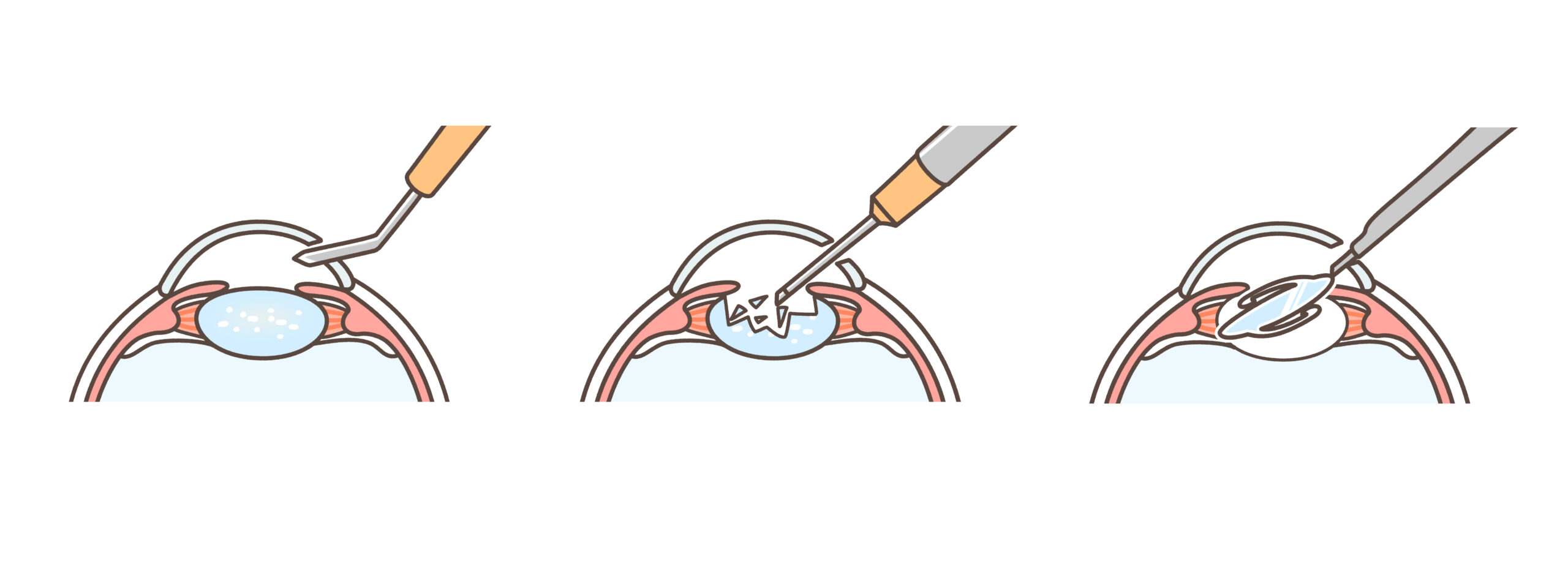
A small incision is made on the side of the cornea, the clear dome-shaped surface that covers the front of the eye.
Dr. Affleck then inserts a tiny probe into the eye. This device emits ultrasound waves that soften and break up the lens so that it can be removed by suction.
This procedure is one of the latest techniques and most common in cataract surgery today. It is called phacoemulsification, also known as “small Incision cataract surgery.”
After the natural lens has been removed, it is replaced by an artificial lens, called an intraocular lens (IOL). An IOL is a clear, acrylic or silicone lens that requires no care and becomes a permanent part of your eye. Light is focused clearly by the IOL onto the retina, improving your vision. You will not feel or see the new lens.
You will need to fast before the surgery, this means “No Food Or Drink After Midnight Before Surgery.” Because you will have sedation, you will need a driver to take you home.
Numbing eye drops and other light sedation will be administered to you before your surgery.
An incision, or opening, is then made in the eye. It is so small no stitches are required to close it. Next the natural lens in your eye will then be removed with a technique called phacoemulsification, which uses a ultrasonic probe to break the lens up into small pieces. Next, these pieces are gently suctioned out of your eye. After your natural lens is removed, the IOL is placed inside your eye. You will want to speak to Dr. Affleck about your IOL options. Dependency on glasses or contacts will normally be determined by the type of IOL the patient selects.
Your eye will be examined the day after surgery by Dr. Affleck, and then at intervals determined by Dr. Affleck. During the immediate recovery period, you will place over the counter lubrications drops in your eyes as needed. The medication Dr. Affleck placed in your eye during surgery my cause a little blurriness for about 2 to 4 weeks, depending on your individual rate of healing. If you have chosen monovision or a multifocal IOL to reduce your dependency on glasses or contacts, they may still be required either for further improvement in your distance vision, reading vision, or both. You should be able to resume your normal activities within 2 or 3 days, and your eye will usually be stable within 3 to 6 weeks. Some individuals may take up to three months. When Dr. Affleck feels healing is satisfactory, glasses or contact lenses could be prescribed if needed.
First, visually Dr. Aaron Affleck must detect the cataracts when he performs a dilated eye exam.
Second, your vision must be affected. This means even with corrective lenses (glasses or contacts) you are unable to see 20/20.
Third, having issues with glare / bright lights.
Fourth, you must have a “complaint of lifestyle.” This means you must state “how the cataract has impacted your life.” The most common is difficulty driving.

For most people cataracts (the forming of clouding lenses inside the eye) starts around age fifty. It is said “If you live long enough you will develop cataracts.” For many individuals, cataract surgery is an opportunity! Enhance your vision, with little to no dependency on corrective lenses along with a large range of focus. Join thousands who have unlocked the secrets of cataracts and seized this once-in-a-lifetime benefit.
After the surgery and a rest, most patients can return to light activity. Some will even elect to drive to the next day appointment. Remember while this is a common result of surgery. It may not happen to you. Please be prepared to take off a week of work, labor and etc. if needed.
Cataract surgery has several steps from the first exam and consult with Dr. Affleck to the last post operative care appointment. If you schedule at the time of your first exam and use the common timeline you will need to see Dr. Affleck often for at least three more exams and two surgeries. The average time table is 3-5 weeks.
By law all testimonials must have disclosures of relationship and sponsorship. Please click here to learn more ♦This testimonial was given by a family member or close friend. For more details contact Stephanie at 208-523-6868